From breath to better care: Shaping the future of COPD monitoring
Chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide and has a profound impact on daily life. Beyond the chronic symptoms, sudden flare-ups, known as exacerbations, are particularly distressing. These episodes often lead to hospitalisations, accelerated loss of lung function, and a significant emotional and economic burden for patients and their families. One of the biggest challenges in COPD care today is recognising exacerbations early enough to take action and mitigate these attacks.
A recently published study in the Journal of Medical Internet Research, led by Atena Mahboubian and colleagues at Leiden University Medical Center (LUMC), sheds new light on this challenge. The research is part of Breath-Sense, a Pathfinder project funded by the European Union, in which RespiQ, LUMC, SINTEF, King’s College London, and uRoboptics collaborate to advance breath-based and remote patient monitoring (RPM) for the management of COPD exacerbations.
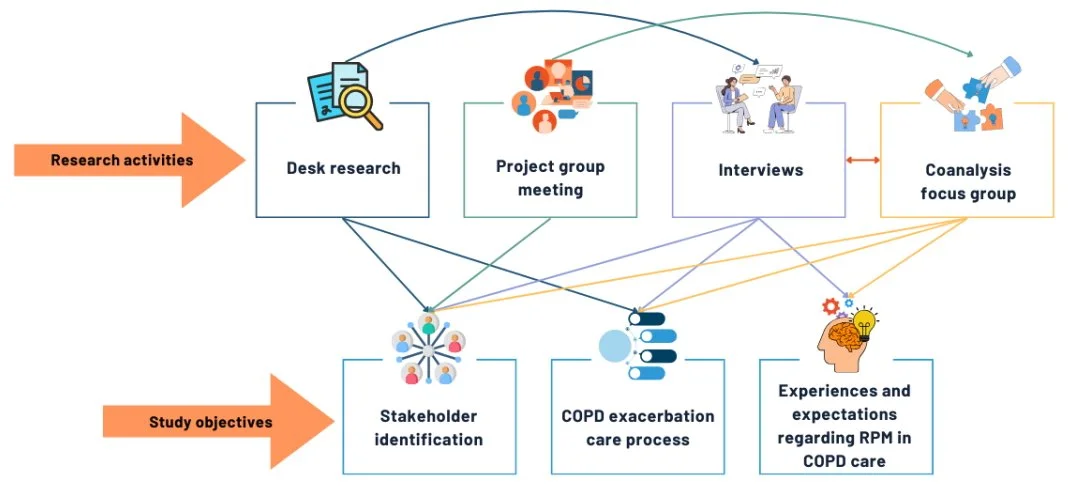
In this study, LUMC researchers carried out a contextual inquiry to lay the foundation for the ongoing cocreation process—a cornerstone of RespiQ’s breath analyser development. The work focused on understanding current COPD exacerbation care, identifying key stakeholders, and exploring their experiences and needs concerning RPM. The insights gained from this process will ensure that future technology development is closely aligned with real-world clinical practice and end-users’ perspectives.
Why early detection of COPD exacerbations matters
The onset of COPD exacerbations is often difficult to determine. In many cases, subtle physiological changes begin days before symptoms become severe. Yet, patients struggle to distinguish between normal day‑to‑day fluctuations, a common cold, and the early stages of an exacerbation. By the time problems are recognised, medical care is often delayed, and the lung attack is already at an advanced stage, making prevention no longer possible.
Early recognition is crucial. Acting sooner can help preserve lung function, reduce hospital admissions, and improve quality of life. This is where RPM has long promised value. Yet, existing solutions have clear limitations.
The limits of current remote monitoring approaches
Most RPM systems used in COPD today rely heavily on questionnaires and self‑reported symptoms, sometimes combined with measurements such as oxygen saturation or physical activity. While helpful for some patients, these approaches are far from perfect.
In their study, the LUMC researchers found that:
Patients often find questionnaires repetitive or hard to interpret.
Subtle changes may go unnoticed if measurements are taken only weekly or monthly.
Healthcare professionals lack objective, early indicators that reliably signal an upcoming exacerbation.
As a result, many patients and clinicians question whether current RPM solutions truly help to detect exacerbations earlier, despite valuing the reassurance and improved communication that these systems can provide.
Breath analysis: A new direction in COPD monitoring
This is where RespiQ’s breath analyser technology comes in.
The paper describes the development of our non‑invasive breath analysis device designed to support COPD exacerbation management. Instead of relying solely on symptoms or questionnaires, RespiQ’s device focuses on breath biomarkers: specific volatile organic compounds (VOCs) present in exhaled breath.
Changes in these biomarkers may occur before patients feel noticeably worse. By measuring patterns in exhaled breath, the technology aims to create a personalised “breath print” that can indicate when an exacerbation may be developing. The current research focuses on understanding how such a technology could be meaningfully integrated into real‑world COPD care.
Cocreation at the core: Listening before building
A key strength of the study is its cocreation approach. Instead of developing technology in isolation, the researchers actively involved those who would ultimately use it and other relevant stakeholders, such as hospital policy advisors.
Through interviews, focus groups, and collaborative analysis sessions, the study gathered perspectives from:
People living with COPD
Pulmonologists and general practitioners
Nurses, physiotherapists, and informal caregivers
Hospital policy advisors
The message was clear: technology alone is not enough. Any successful solution must fit seamlessly into existing care pathways, support–rather than replace–human interaction, and be accessible to patients with different levels of health literacy and digital skills.
The cocreation journey behind the study, illustrating how patient input and clinical expertise were combined to guide the development of future remote monitoring solutions for COPD.
What patients and clinicians really want
Participants in the study expressed cautious optimism about remote monitoring and breath‑based technologies.
Patients liked the idea of a system that could “keep an eye on them” and potentially detect problems earlier, especially if it reduced uncertainty and anxiety. At the same time, they stressed that they did not want care to become impersonal or overly data‑driven.
Healthcare professionals saw clear potential value in objective, continuous measurements that complement clinical judgement and patient‑reported symptoms. Many highlighted that breath analysis could help bridge a critical gap: the period before symptoms become severe enough to trigger action.
How RespiQ fits into the future of COPD care
By focusing on non‑invasive, breath‑based monitoring, RespiQ represents a promising shift in how COPD exacerbations might be managed in the future. Rather than reacting to worsening symptoms, care could become more proactive, supporting earlier conversations, timely interventions, and better‑informed decisions.
This insightful study lays out the groundwork for what comes next: refining the technology, defining clear care processes, and continuing to involve patients and professionals along the way.
This approach reflects a broader trend in healthcare innovation: building solutions with users, not just for them.
Looking ahead
COPD is a complex condition, and no single tool will solve all its challenges. However, the combination of scientific research, user-centred design, and innovative technologies like RespiQ’s breathalyser opens exciting possibilities.
Looking forward, the next phase will focus on defining the needs, values, and requirements of both patients and healthcare professionals. Together with them, we will co-develop and refine a prototype that will be tested in think-aloud or other interactive sessions.
As development unfolds, breath analysis may become a valuable addition to COPD care, helping patients feel more secure, supporting clinicians with objective insights, and ultimately improving outcomes in a disease where timing truly matters.
Reference: Mahboubian A, Kasteleyn M, Bašić E, Chavannes N, Aardoom J. Patients’ and Health Care Professionals’ Perspectives on Remote Patient Monitoring in Chronic Obstructive Pulmonary Disease Exacerbation Management: Initiating Cocreation. J Med Internet Res 2025;27:e67666. URL: https://www.jmir.org/2025/1/e67666. DOI: 10.2196/67666
Written by Laura Verga, 16/12/2025
Reviewed by Atena Mahboubian, Marise Kasteleyn, Jiska Aardoom, 06/01/2026